How much do you know about your anatomy? What is really considered normal? Should we even say that something is “normal?” Well with this series of blog posts, I hope to dispel some of the myths about female anatomy, as well as discuss certain changes in pelvic anatomy that would warrant a visit to your gynecologist.
As always, this post does not take the place for actual medical advice. If you have concerns or questions, please reach out to your provider. That said, to the vulva!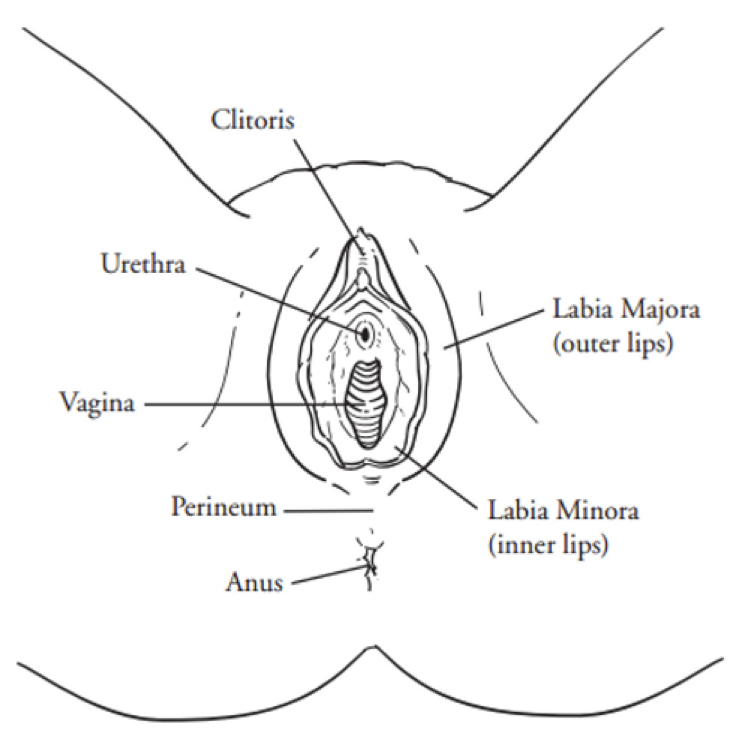
This is a very black and white, textbook illustration of the external female genital tract. I would be remiss if I didn’t point out that the vagina is only a small part of this entire structure. As a society, we colloquially refer to the female genitalia as the “vagina” for some reason, but in reality it is a very specific section. More on that later..
This week, we’ll be starting from the top. I present to you…
THE CLITORIS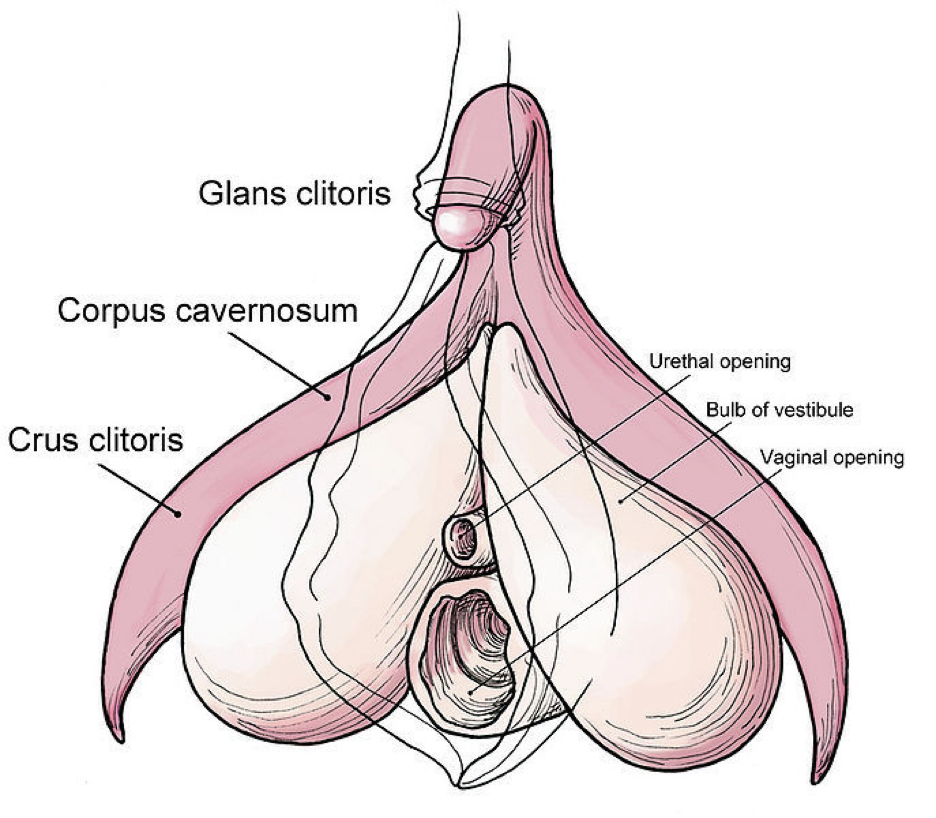
This is an impressive structure. If you know anything about male anatomy, you will see some correlations in the names of certain structures, namely the corpus cavernosum, as well as the glans. This is because the clitoris is what is considered an anatomic homologue, a structure that has a equivalent in the opposite biologic sex. The crazy thing about the clitoris is that it has only recently been fully examined in terms of innervation, vascularity, and structure, and by recently I mean since the 90’s (with most articles published after 2000). This journal article, which was published in 2005, is one of the first to fully “…present a comprehensive account of clitoral anatomy, including its component structures, neurovascular supply, relationship to adjacent structures (the urethra, vagina and vestibular glands, and connective tissue supports), histology and immunohistochemistry.”
Just for reference, I was in medical school in 2005 and “Holla Back Girl,” was resting at #2 on the Billboard Hot 100 list.
I would also point out that the article discussed above was published in a Urology journal, not Gynecology. This is a huge issue, because as gynecologists, we are supposed to be THE expert in female anatomy. To compound things even further, until very recently, no gynecologic textbooks mentioned specifics about clitoral anatomy (length of nerves, vascular compliance, etc.). As to why this is…well, that’s a great question. Maybe it’s due to what Jessica Pin, (one of the lead authors of the study that pushed detailed clitoral anatomy into certain GYN textbooks) reported as “…sociocultural discomfort with the clitoris and a pervasive lack of regard for female sexual response (seen as a bonus rather than necessity), as it is not legitimized by direct reproductive function.” Maybe it’s a decision of whom Dr. Jen Gunther calls the “Patriarchy,” the oppressive consortium of medical policy makers that define what is, and what is not, important in women’s health. Or maybe it’s simply an oversight on the part of medical textbooks editors and physician educators for the last, oh, 1000 years?
Regardless, the clitoris has an important role in women’s sexual health, and overall sense of wellbeing. It is, therefore, incredibly important for women’s health providers to understand the anatomy, as well as function of the clitoris, especially in patients that present with complaints regarding that organ.
What are some of those complaints, you ask? Well, here is small collection of common clitoral concerns!
Clitorodynia: An overarching term that basically means pain in the clitoris. Clitorodynia may be due to clitoral adhesions, vascular insufficiency, keratin pearls, neuropathies, or a multitude of other conditions.
Clitoral Adhesions: Clitoral adhesions are scar-like tissue formations that form between the glans of the clitoris and the clitoral hood. This may lead to tenderness or itching in the clitoral area, and can be a cause of painful intercourse, pelvic pain, or even Persistent Genital Arousal Disorder (PGAD). In certain cases, these adhesions can lead to the formation of small keratin collections called keratin pearls.
Clitoral Retraction: Clitoral retractions may occur with conditions that cause sex hormone level to be low, such as menopause or long-term oral contraceptive use, or in vulvar skin conditions such as lichen sclerosus. A retracted clitoris can be tender, and may lead to significant discomfort with sexual activity.
Clitoral Itching: Often associated with vulvar dermatoses, clitoral itching can be a symptom of multiple conditions, including cancer of the clitoris itself. Persistent clitoral itching, as with any type of persistent genital itching, should be investigated.
Well friends, that’s all I have for you today. I hope you enjoyed the first of this blog series. As always if you have any questions or concerns, please let me know.
Have a wonderful rest of your day, and remember – there is hope, there is help, there is Haven Center!