Understanding Low Sexual Desire: What You Need to Know
If you’ve ever struggled with a lack of sexual desire, you’re definitely not alone. In fact, concerns about sexual desire are among the most common reasons women visit a sexual medicine clinic. Some studies show that up to 48% of female patients with sexual dysfunction report low desire. With numbers like that, it’s clear how important it is to understand what’s going on when desire drops, how to diagnose the underlying causes, and, of course, what can be done to treat it.
But here’s the thing—when someone comes in saying they have low desire, it’s not always the main issue. Often, there could be other factors at play, like pain during sex or vaginal dryness, and the low desire is just a symptom of those bigger concerns. So, when it comes to addressing low libido, we have to think about all the pieces of the puzzle.
What Exactly is Sexual Desire?
Let’s start with the basics: sexual desire is the feeling or motivation to engage in sexual activity, whether with a partner or solo. You might hear people refer to it as “libido” or “sex drive.” Sometimes, it’s even mixed up with getting “turned on,” but that’s more about arousal, which comes later in the process. Sexual desire is more like the mental and emotional drive to be sexual in the first place.
Interestingly, sexual desire comes from the brain, not just from hormones or external factors. It’s primarily driven by brain activity from the nucleus accumbens (NA) and the ventral tegmental area (VTA), which are involved in our reward system – meaning they help regulate pleasure and motivation. Dopamine, which is one of the key players in the brain’s reward system, is closely linked to sexual desire, and this is where testosterone comes in—testosterone helps boost dopamine, which is why it’s connected to libido!
But it’s not just biology driving desire. There’s also a psychological and social aspect—which we think of as a biopsychosocial triad. This means that your feelings about sex, your relationship status, and even societal views on sexuality can influence how you experience desire. These three factors—biological, psychological, and social—are like the legs of a stool. If one leg is wobbly or missing, the whole thing can collapse.
Why Do We Have Sexual Desire?
From an evolutionary point of view, sexual desire helps ensure the survival of the species. Just like hunger makes us seek food, sexual desire pushes us to engage in activities that lead to reproduction. But desire isn’t only about making babies, it has other functions, too. During sexual activity, especially with orgasm, the body releases hormones like oxytocin and dopamine. These “feel-good” hormones act on the brain’s reward system, creating that sense of pleasure and satisfaction. They essentially tell your brain, “Hey, that was fun. Let’s do it again!” Interestingly, oxytocin is also a natural pain reliever, which may explain why some people seek sexual activity to alleviate discomfort.
What Factors Affect Female Sexual Desire?
There’s no single answer to why someone may experience a drop in sexual desire—there are many factors at play. Some common ones include relationship dynamics, levels of sexual satisfaction, personal health, and even your own feelings about sex. Research has shown that patients with high levels of satisfaction in both partnered and solitary sexual activity tend to report higher overall desire. In other words, if you’re enjoying sex—whether with a partner or on your own—you’re more likely to want to keep doing it.
Here’s a quick look at some of the top factors that influence sexual desire:
- For partnered (dyadic) sexual desire, things like your level of satisfaction, your partner’s interest in sex, and how much you love your partner can play big roles.
- For solitary sexual desire, factors like whether you’ve masturbated recently, your age, and your desire for partnered sex also make a difference.
Interestingly, while romantic love does factor into sexual desire, it’s not the biggest influence. Satisfaction with the sexual experience itself is more important, whether it’s with a partner or solo.
When Does It Become a Problem?
Not everyone with low sexual desire has a problem. Sexual desire is very personal, and what’s “normal” can vary a lot from one person to another. Low sexual desire only becomes an issue when it causes distress. So, if someone’s not bothered by having less desire, it’s not necessarily a problem that needs fixing.
One challenge in diagnosing sexual desire disorders is figuring out whether the issue is related to partnered or solitary sexual activity. For example, someone might be perfectly happy with their level of partnered sexual activity but feel frustrated by a lack of desire for solo sex—or vice versa. Understanding this distinction can help healthcare providers get to the root of the issue and recommend the best treatment options.
How Can It Be Treated?
When a patient comes to the clinic with concerns regarding low sexual desire, our first step is figuring out what may be causing that concern. This usually involves taking a thorough medical history to rule out things like hormonal imbalances or medications that could be affecting libido. A physical exam can also help identify any underlying issues, such as pain or vaginal dryness, that might be impacting desire. Lastly, it’s essential to explore psychological and relational factors—everything from stress to relationship issues to personal attitudes about sex.
Treatment will depend on what’s causing the low desire. For some women, hormone therapy, especially testosterone or estrogen therapy, might help. For others, addressing psychological factors through therapy or counseling may be more effective. There are also medications designed to increase sexual desire, but these should be used alongside other treatments that address the emotional and relational aspects of the issue.
In Conclusion
Low sexual desire is complex, with many factors contributing to how and why it happens. While it’s one of the most common concerns brought to sexual medicine clinics, it’s important to remember that desire is highly individualized. What matters most is how the woman feels about her level of desire—if it’s causing distress, then it’s worth addressing. By looking at all the different aspects of desire, healthcare providers can create a treatment plan that helps women feel better, both physically and emotionally.
Do have concerns about low sex drive? Call our office today and let’s get your desire where you want it to be!



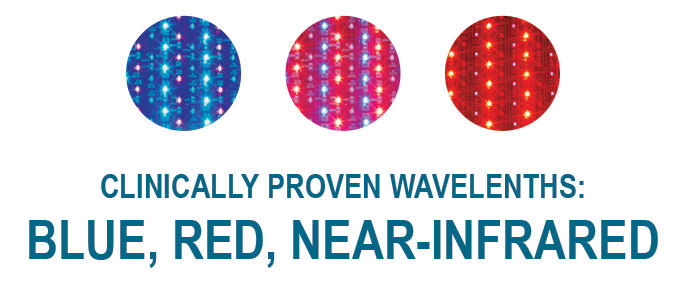
 At the heart of Celluma lies a matrix of light-emitting diodes (LEDs) that emit specific wavelengths of light, including blue, red, and near-infrared. Each wavelength penetrates the skin at varying depths, targeting different cellular processes.
At the heart of Celluma lies a matrix of light-emitting diodes (LEDs) that emit specific wavelengths of light, including blue, red, and near-infrared. Each wavelength penetrates the skin at varying depths, targeting different cellular processes.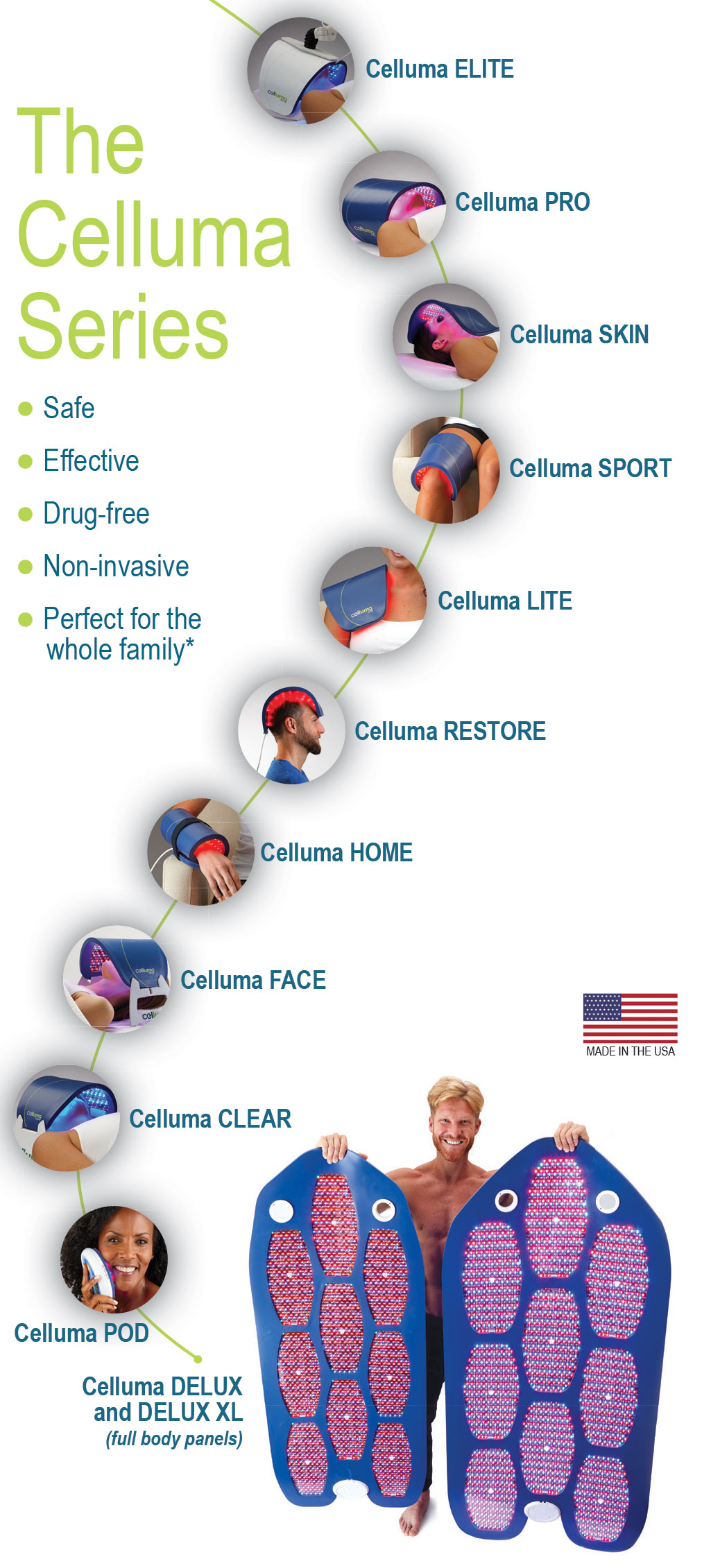 Skin Rejuvenation: Celluma Light Therapy offers a non-invasive alternative to traditional skincare treatments. By stimulating collagen production and improving cellular function, it diminishes fine lines, wrinkles, and age spots, resulting in a more youthful complexion.
Skin Rejuvenation: Celluma Light Therapy offers a non-invasive alternative to traditional skincare treatments. By stimulating collagen production and improving cellular function, it diminishes fine lines, wrinkles, and age spots, resulting in a more youthful complexion.